Periodontitis, a severe form of gum disease, poses a significant threat to oral health, potentially leading to tooth loss and other complications if left untreated. This article delves into the causes, symptoms, prevention, and treatment of periodontitis to help individuals better understand and address this common dental concern.
What is Periodontitis
Periodontitis is an advanced stage of gum disease characterized by inflammation of the structures surrounding the teeth. It often originates from untreated gingivitis, where bacterial plaque buildup on teeth triggers inflammation of the gums. As periodontitis progresses, it can lead to the formation of pockets between the teeth and gums, which become breeding grounds for bacteria.
the common causes of periodontitis:
1. Poor Oral Hygiene:
Inadequate brushing and flossing allow plaque—a sticky film of bacteria—to accumulate on teeth. Over time, this plaque hardens into tartar, leading to inflammation of the gums, the initial stage of gum disease (gingivitis), which can progress to periodontitis if not addressed.
2. Smoking:
Tobacco use, particularly smoking, is a significant risk factor for periodontitis. Smoking weakens the immune system, making it harder for the body to fight off infections, including those affecting the gums.
3. Genetics:
Genetic factors can influence an individual’s susceptibility to gum disease. Some people may be genetically predisposed to develop periodontitis, even with good oral hygiene practices.
4. Diabetes:
Individuals with diabetes are at an increased risk of developing periodontitis. The fluctuating blood sugar levels associated with diabetes can impair the body’s ability to combat infections, including those affecting the gums.
5. Hormonal Changes:
Hormonal fluctuations, such as those during pregnancy, menstruation, and menopause, can affect the gums. This makes women more susceptible to gum disease during certain life stages.
6. Certain Medications:
Some medications, like certain antihypertensive drugs and anticonvulsants, can contribute to gum tissue changes, making it easier for bacteria to cause inflammation and infection.
7. Immune System Compromises:
Conditions or medications that compromise the immune system, such as HIV/AIDS or immunosuppressive drugs, increase the risk of infections, including those affecting the gums.
Recognizing the Symptoms:
1. Red, Swollen Gums:
• Explanation: Inflammation is a key sign of gum disease. Healthy gums should appear pink and firm, not red and swollen. 
2. Bleeding During Brushing or Flossing:
• Explanation: Bleeding gums indicate inflammation. Healthy gums should not bleed during regular oral hygiene practices.
3. Persistent Bad Breath:
The buildup of bacteria in the mouth produces toxins that contribute to bad breath, a common symptom of gum disease.
4. Receding Gums:
Gums that are pulling away from the teeth can create pockets where bacteria thrive, leading to further infection. 
5. Changes in Tooth Alignment:
As periodontitis progresses, teeth may shift or become loose due to the destruction of supporting structures.
Prevention Strategies
Practicing good oral hygiene is the primary line of defense against periodontitis. Regular brushing with fluoride toothpaste, flossing to remove plaque between teeth.
Routine dental check-ups for professional cleanings are essential preventive measures.
Lifestyle changes, such as quitting smoking.
Maintaining a balanced diet, also contribute to overall oral health.
Professional Treatment
Dentists employ various approaches to address periodontitis, depending on its severity. Professional dental cleanings remove accumulated plaque and tartar. Scaling and root planing, a non-surgical procedure, involve cleaning the infected root surfaces to encourage healing. In advanced cases, surgical interventions like flap surgery or bone grafts may be necessary to restore oral health. 
Home Care for Periodontitis Management
1. Saltwater Rinse:
• How to: Mix a teaspoon of salt in a glass of warm water. Rinse your mouth with this solution after brushing to help reduce inflammation and promote healing.
2. Oil Pulling:
• How to: Swish a tablespoon of coconut oil or sesame oil in your mouth for about 15-20 minutes before spitting it out. This practice is believed to help reduce bacteria and improve gum health. 
3. Green Tea:
• How to: Drink green tea, which contains antioxidants that may help reduce inflammation and fight bacteria. You can also use a cooled, used tea bag as a compress on affected areas. 
4. Aloe Vera Gel:
• How to: Apply a small amount of pure aloe vera gel to your gums. Aloe vera has anti-inflammatory properties that may help soothe irritated gums.

5. Turmeric Paste:
• How to: Mix turmeric powder with water to form a paste. Apply this paste to your gums and leave it for a few minutes before rinsing. Turmeric has anti-inflammatory and antimicrobial properties. 
6. Probiotics:
• How to: Consume foods rich in probiotics, like yogurt with live cultures. Probiotics can contribute to a healthier balance of bacteria in the mouth. 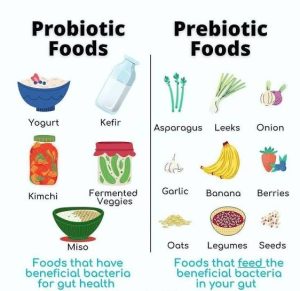
Periodontitis is a serious dental condition that demands attention and proactive care. By understanding its causes, recognizing symptoms, and embracing preventive measures, individuals can significantly reduce the risk of developing this advanced gum disease. Early intervention and a commitment to good oral hygiene are key to preserving oral health, ensuring a vibrant smile, and preventing the potentially severe consequences of untreated periodontitis. Regular dental check-ups remain a cornerstone in the battle against gum disease, promoting a lifetime of healthy smiles
Stay tuned for more updates.