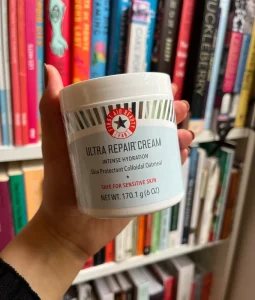
First aid beauty ultra repair. Although some consumers have complained that First Aid Beauty Ultra Repair Cream is not appropriate for sensitive or acne-prone skin, the product is generally praised for its calming and hydrating qualities, especially for dry and sensitive skin. It is commended for its whipped, non-greasy texture and for its capacity to hydrate skin both immediately and over time, leaving it feeling pleasant and smooth. Ceramides, shea butter, and colloidal oatmeal are important components.
FIRST AID BEAUTY ULTRA REPAIR
For many, its overall performance and calming qualities make it a good investment, even though its rich texture might not be to everyone’s taste, especially for those with oily skin. The significant advantages it provides outweigh any possible disadvantages, such as pricing and packaging preferences. First Aid Beauty Ultra Repair Cream is a great option for people who want to treat extreme dryness and skin irritation with a product that provides both short-term and long-term comfort.
Formulation and Ingredients;

First Aid Beauty (FAB) Ultra Repair Cream is celebrated for its rich, emollient formula that is designed to deliver intense hydration and soothe distressed skin. Key ingredients include:
1. Colloidal Oatmeal: Renowned for its anti-inflammatory properties, colloidal oatmeal helps soothe and calm irritated skin.
2. Shea Butter: A deeply nourishing ingredient that provides essential fatty acids and vitamins, aiding in skin barrier repair and hydration.
3. Allantoin: Known for its skin-soothing properties, allantoin helps to calm and protect the skin.
4. Glycerin:: A powerful humectant that draws moisture into the skin, ensuring prolonged hydration.
5. Ceramides: Essential for maintaining the skin’s barrier function, ceramides help to lock in moisture and protect against environmental aggressors.
This blend of ingredients makes the it suitable for a wide range of skin types, including sensitive and eczema-prone skin.
Effectiveness;

FIRST AID BEAUTY ULTRA REPAIR
Users have consistently reported significant improvements in skin hydration, texture, and overall comfort after incorporating FAB Ultra Repair Cream into their routines. The cream’s thick, emollient texture is particularly effective for dry, flaky skin, providing immediate relief and lasting moisture.
Clinical studies and user testimonials highlight the cream’s effectiveness in treating conditions like eczema and dermatitis. The inclusion of colloidal oatmeal and shea butter provides both immediate and long-term benefits, reducing redness and irritation while enhancing the skin’s natural barrier.
Benefits;

FIRST AID BEAUTY ULTRA REPAIR
1. Intense Hydration: The rich formula provides deep, lasting moisture, making it ideal for very dry and dehydrated skin.
2. Soothing Properties: Ingredients like colloidal oatmeal and allantoin help to calm and soothe irritated or inflamed skin.
3. Multi-purpose Use: Suitable for face and body, the Ultra Repair Cream offers versatility in skincare routines.
4. Hypoallergenic: Free from harsh chemicals and common allergens, it is designed to be safe for sensitive skin.
5. Immediate Relief: Provides quick relief for dry, itchy skin, making it a staple for those with chronic dryness or skin conditions.
Potential Drawbacks;

FIRST AID BEAUTY ULTRA REPAIR
1. Rich Texture: While beneficial for very dry skin, the thick texture might feel too heavy for those with oily or combination skin.
2. Packaging: The cream is often packaged in jars, which some users find less hygienic compared to pump dispensers.
3. Price Point: Although effective, FAB Ultra Repair Cream is relatively more expensive compared to other over-the-counter moisturizers.
Summary
Particularly for people with dry, sensitive, or irritated skin, it has established itself as a skincare must. This review gives prospective users a thorough overview by exploring its formulation, advantages, efficacy, and possible disadvantages.