
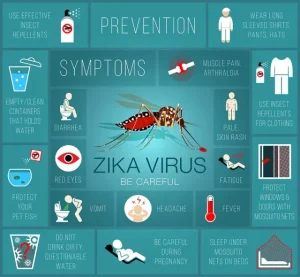
What is zika virus?. The virus is a mosquito-borne disease that usually has little to no symptoms, but it can cause major birth problems like microcephaly if it is transferred from a pregnant mother to her fetus. It can be transferred through intercourse and by the bite of an infected Aedes mosquito. Pregnant women should take extra care in areas that are impacted, even if symptoms including fever, rash, joint discomfort, and conjunctivitis are usually minor and temporary.
WHAT IS ZIKA VIRUS?
Because of its potential to cause serious birth abnormalities and neurological disorders, the Zika virus continues to be a major public health issue. People can lower their risk of infection by being aware of the ways in which the disease is spread, identifying symptoms, and taking precautions. In order to stop the Zika virus from spreading and to safeguard vulnerable groups, especially expectant mothers and their unborn children, public health initiatives and community awareness are essential.
Transmission;
The Zika virus is primarily spread through the bites of infected Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. These mosquitoes are most active during the daytime, especially in tropical and subtropical regions. In addition to mosquito bites, Zika can be transmitted through:
– Mother-to-Child: During pregnancy, the virus can be passed from an infected mother to her fetus, potentially causing birth defects.
– Sexual Contact: The virus can be transmitted through sexual intercourse with an infected person.
– Blood Transfusion: Though rare, Zika can be transmitted through blood transfusions from infected donors.
Zika virus Symptoms;

WHAT IS ZIKA VIRUS?
Many people infected with the Zika virus do not exhibit symptoms. When symptoms do occur, they are usually mild and can last for several days to a week. Common symptoms include:
– Fever
– Rash
– Joint pain
– Conjunctivitis (red eyes)
– Muscle pain
– Headache
The major concern with Zika virus infection is its impact on pregnancy. Infection during pregnancy can lead to severe birth defects, including microcephaly, a condition where babies are born with abnormally small heads and underdeveloped brains. Other neurological complications have also been associated with Zika, such as Guillain-Barré syndrome.
Prevention;
WHAT IS ZIKA VIRUS?
Preventing this infection primarily involves avoiding mosquito bites and practicing safe behaviors. Key preventive measures include:
– Use Insect Repellents: Apply repellents containing DEET, picaridin, or oil of lemon eucalyptus to exposed skin.
– Wear Protective Clothing: Wear long-sleeved shirts, long pants, socks, and shoes to minimize skin exposure.
– Eliminate Standing Water: Regularly empty and clean containers that hold water, such as flower pots, buckets, and birdbaths, to reduce mosquito breeding sites.
– Use Mosquito Nets: Sleep under mosquito nets, especially in areas with high Zika transmission rates.
– Install Screens: Ensure that windows and doors have screens to prevent mosquitoes from entering indoor spaces.
– Safe Sex Practices: Use condoms or abstain from sex to reduce the risk of sexual transmission, especially if your partner has traveled to or resides in an area with active transmission.
Treatment;

WHAT IS ZIKA VIRUS?
There is no specific antiviral treatment for this infection. Treatment focuses on relieving symptoms and includes:
– Rest: Ensure plenty of rest to help the body fight the infection.
Summary
Due to its rapid spread and significant health risks, especially for expectant mothers and their unborn children, the Zika virus has drawn attention from all around the world. A serious threat to public health, it is mostly carried by Aedes mosquitoes, which are also the vectors of dengue and chikungunya.