MESOTHELIOMA
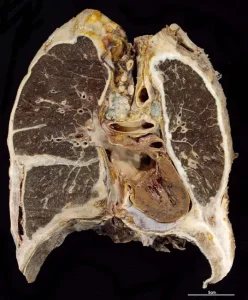
Mesothelioma. Immunotherapy, chemotherapy, radiation, targeted therapy, and surgery are some of the treatments for mesothelioma, a rare cancer that most often begins in the lining surrounding your lungs but can also begin in the lining or sac surrounding your abdomen, heart, or testicles. Symptoms include shortness of breath, coughing, night sweats, chest pain, and digestive problems
MESOTHELIOMA
Your mesothelium, a sort of tissue that forms the lining that envelops and shields specific organs, is where it begins. It frequently produces many tumors, which can occasionally group together to form a layer over the afflicted organs, making treatment challenging.
Types

pleural mesothelioma is the most prevalent kind of it, affecting the lining of the lungs. Other varieties consist of:
Mesothelioma peritoneal. The lining of your pelvic and abdominal cavities is impacted. It is mesothelioma’s second most prevalent form.
heart-related mesothelioma. Your heart’s sac is impacted by this. It’s really uncommon.
Paratesticular mesothelioma pertains to mesothelioma of the tunica vaginalis testis. The lining surrounding your testicles is impacted by this. It’s really uncommon as well.
Although they are not closely connected to malignant (cancerous) mesothelioma, isolated fibrous tumors are occasionally referred to as “benign mesothelioma.”
Symptoms

The location of mesothelioma in your body determines its symptoms. Among them are:
Fever
Sweating at night
Fatigue
Unintentional weight loss
Abdominal or chest pain
respiratory symptoms, such as coughing, dysphagia (difficulty swallowing), and worsening dyspnea
Diarrhea, appetite loss, nausea, and vomiting are examples of digestive symptoms.
Cardiovascular symptoms, such as irregular heartbeats and low blood pressure
Pain, lumps, or swelling in your groin or scrotum
Causes
The most frequent cause of this is exposure to asbestos. A naturally occurring material, asbestos was previously widely used in a variety of industries, including as shipbuilding, construction, and the automobile sector. It contains needlelike fibers that, if swallowed or inhaled, can harm your tissues. After asbestos exposure, mesothelioma may not appear straight away; it may take decades for the malignancy to manifest.
However, a number of circumstances can influence the development of cancer; most asbestos exposure does not result in mesothelioma. Furthermore, a history of asbestos exposure is not always present in mesothelioma patients.
Treatment

Surgery. Surgery options include cytoreduction, pericardiectomy, pleurectomy with decortication (removing the tumor and your pleura), and extrapleural pneumonectomy.
Immunotherapy. These therapies strengthen your immune system’s capacity to recognize and eliminate cancerous cells.
Chemotherapy. Chemotherapy medications are often administered by an IV, which enters your bloodstream and kills cancer cells. Certain types of chemotherapy, such as hyperthermic intraperitoneal chemotherapy (HIPEC), are administered more directly to the tumor.
targeted treatments. Targeted medicines may be able to treat genetic alterations in your tumor cells.
radiation treatment. High-energy X-rays are used in radiation therapy to kill cancer cells.
clinical experiments. Your doctor may suggest clinical trials for drugs whose efficacy is still being investigated.
palliative care. Palliative care may be suggested by your doctor to help you cope with the side effects of cancer treatment and its symptoms. Procedures to remove fluid from the area surrounding your organs and pain treatment are examples of palliative care types.
Summary
When mesothelioma is diagnosed, many people experience anxiety and uncertainty. Knowing what’s ahead and having a clear path to follow are natural desires. You may find it useful to locate support groups and other services that can help you understand your options and provide assistance. Talk openly with your provider about your particular circumstances, your worries, and your expectations.