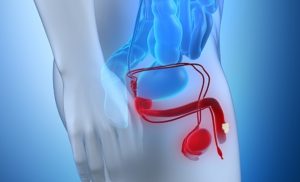
PENILE CANCER
Penile cancer. When your penis’s healthy cells alter and proliferate uncontrollably, penile cancer results. The rod-shaped reproductive organ that enables urination and sexual activity is your penis. It consists of the glans, a rod-like region (shaft) that runs from your low abdomen to the tip of your penis. The foreskin is a layer of skin that covers the head if you are not circumcised. Your penis’ head is visible if you have had circumcision.
PENILE CANCER
Cancer can develop anywhere in the penis, but if you are not circumcised, it usually begins on the head or foreskin. Penile cancer, a relatively uncommon cancer of the penis, is frequently a squamous cell carcinoma, originating from the skin cells. Uncircumcision, HPV infection, smoking, and poor hygiene are risk factors. Successful treatment, which may include chemotherapy, radiation, or surgery, depends on early detection.
Types

SCC stands for squamous cell cancer. The epithelium, the outermost layer of your skin, is where this cancer develops. 95% of all penile malignancies are of this type.
Melanoma. Melanocytes, the cells that regulate how dark or light your skin is, are where this type of cancer starts. A more aggressive type of cancer is melanoma.
BCC, or basal cell cancer. The lowermost layer of your epithelium is where the cancer starts. BCC is a type of penile cancer that grows slowly.
Adenocarcinoma. Your glandular cells, which produce perspiration, mucus, and other bodily fluids, are where this cancer begins.
cancer of the urothelium. The urothelium, the tissue lining your bladder, kidneys, and other urinary system organs, is where this cancer develops.
Sarcoma. Muscle or connective tissue is where this kind of cancer first appears.
Signs

Not every cancer results in visible alterations. However, penile cancer typically results in a change in the appearance of your penis. There may be a lump and discoloration of the skin on your penis.
Symptoms of penile cancer include:
A sore or bump that doesn’t hurt and could leak
Flat growths with a blueish-brown appearance
Something that smells bad beneath your foreskin Rash
Skin thickening or color change
little, crusty lumps
inflammation and swelling, particularly in the penis’ head (balanitis)
These symptoms are sometimes brought on by less serious illnesses including allergies and infections. Don’t leave anything to chance, though. To ensure that early-stage cancer is not left untreated, it is preferable to have a medical professional examine it.
Causes
When healthy cells alter and proliferate uncontrollably, cancer results. However, scientists are unsure of the initial reason of that transformation.
Although they haven’t discovered any reasons, researchers have discovered risk factors.
Treatment

Circumcision. Your doctor might remove the tissue if the cancer is limited to your foreskin.
Cryotherapy. Extreme cold is used in this therapy to kill the tumor.
Excision. Your doctor might remove the tumor or cancerous cells from your penis.
Ablation via laser. In order to eliminate the tumor, this treatment uses lasers that produce extremely high temperatures.
creams with medication. You apply this lotion to your penis on a regular basis. Imiciquimod and fluorouracil are common medications.
Mohs surgery. In order to reach the healthy tissue underlying, your healthcare practitioner will remove the malignant skin layer by layer throughout this treatment.
radiation treatment. Before surgery, your doctor might employ energy beams, such as X-rays, to reduce a tumor or kill cancer cells.
Summary
Receiving a diagnosis of penile cancer is a life-altering event that causes a flurry of feelings and questions. Feeling overburdened is normal and acceptable, so it’s crucial to look after yourself during this time. Consult your physician. In addition to discussing possible treatment choices, they can direct you to resources for both emotional and practical support. Rely on your loved ones and medical team. This is not unique to you.