
PULMONARY HYPERTENSION
Pulmonary hypertension. Your pulmonary arteries. which transport blood with low oxygen content from your heart to your lungs, can become hypertensive. Shortness of breath while your daily activities is the first sign. The most frequent causes are hypoxia, lung illness, and heart disease. Your quality of life may improve with an early diagnosis and course of therapy.
PULMONARY HYPERTENSION
The general diagnosis of pulmonary hypertension (PH) indicates that you have high blood pressure in your pulmonary arteries, which are the blood vessels that transport oxygen-poor blood from your heart to your lungs. There are numerous causes of PH, with heart disease and lung disease being the most common, but a number of other illnesses and environmental factors can also increase your risk for PH. The danger of pulmonary hypertension is that it interferes with the normal flow of blood through your heart and lungs, narrowing the arteries and making it harder for your heart to pump oxygen-poor blood to your lungs.
Symptoms
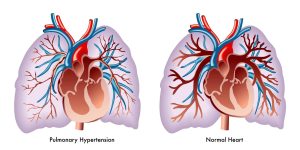
Pulmonary arterial hypertension (PAH) causes group 1 PH. There are numerous causes of PAH, from underlying illnesses to specific medications. Your pulmonary arteries become rigid, thick, or narrow as a result of PAH. Your pulmonary arteries’ pressure rises as less blood can pass through.
Group 2 PH because to cardiac disease on the left side. Your heart’s left side circulates blood throughout your body. Your entire pulmonary circuit and the right side of your heart are impacted if there is an issue with this side of your heart. Your heart backs up with blood, which causes your pulmonary arteries to become more pressurized.
When pulmonary hypertension first strikes, you might not have any symptoms, or if you do, they might be mild. However, as the condition worsens, you may find it more difficult to carry out your daily activities, experience fatigue, feel less hungry than normal, experience pain in the upper right side of your stomach, experience a racing heartbeat, or experience swelling (edema) in your ankles, legs, or stomach.
Stages
Class 1: You are symptom-free.
Class 2: When you’re sleeping, you don’t experience any symptoms. However, while performing certain everyday tasks, you experience some discomfort or dyspnea. These include climbing stairs and doing housework.
Class 3: When you’re sleeping, you might still feel good. However, because you feel exhausted or out of breath, it is now much more difficult to perform daily duties.
Class 4: Even while you’re at rest, you get symptoms. Attempting to perform any routine task exacerbates the symptoms.
Treatment
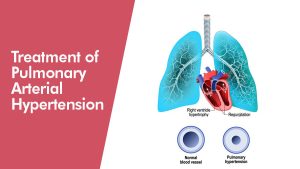
Also, the type of pulmonary hypertension you have and your other health issues will determine how you are treated. Treatment will be customized by your medical team to meet your specific needs.
There are now just two forms of PH that can be directly treated:
PAH, or pulmonary arterial hypertension.
pulmonary hypertension caused by chronic thromboembolism.
In order to treat various forms of PH, the underlying medical issues must be managed.
The following are some methods of treating pulmonary arterial hypertension (PAH):
Blockers of calcium channels. The blood pressure in your pulmonary arteries and throughout your body can be lowered with the aid of these drugs.
Summary
Altough, a diagnosis of pulmonary hypertension might elicit a variety of feelings. Learning what’s happening inside your body, processing the diagnosis, and deciding how to proceed all take time. To obtain the resources you require, collaborate with your provider. Include your friends and family in the adjustments you make to your lifestyle.